7 year old female spayed CKCS we were monitoring for MVD.
In April of 2023, Ginger was staged at B1 MVD with trivial TV regurgitation. MV murmur=3/6
In early September – fever of unknown origin, ocular pain and increased respiratory rate. Blood work revealed a leukocytosis with normal serology. Chest radiographs showed mild cardiomegaly with no left atrial enlargement and no evidence of pulmonary edema. Ocular pressures revealed uveitis of the left eye with normal right IOP. She was placed on a course of Amoxicillin/Clavulinic acid and eye medications for a uveitis.
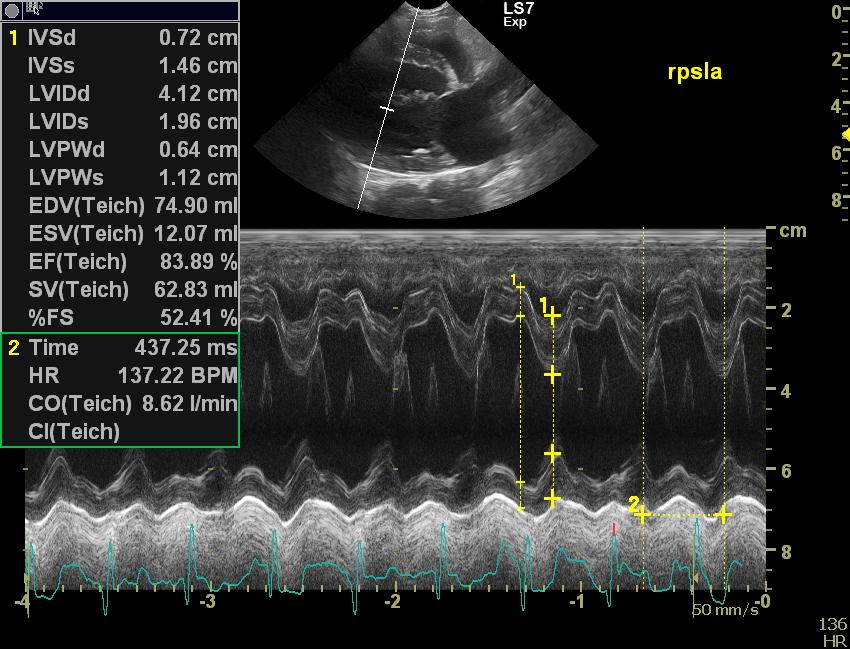
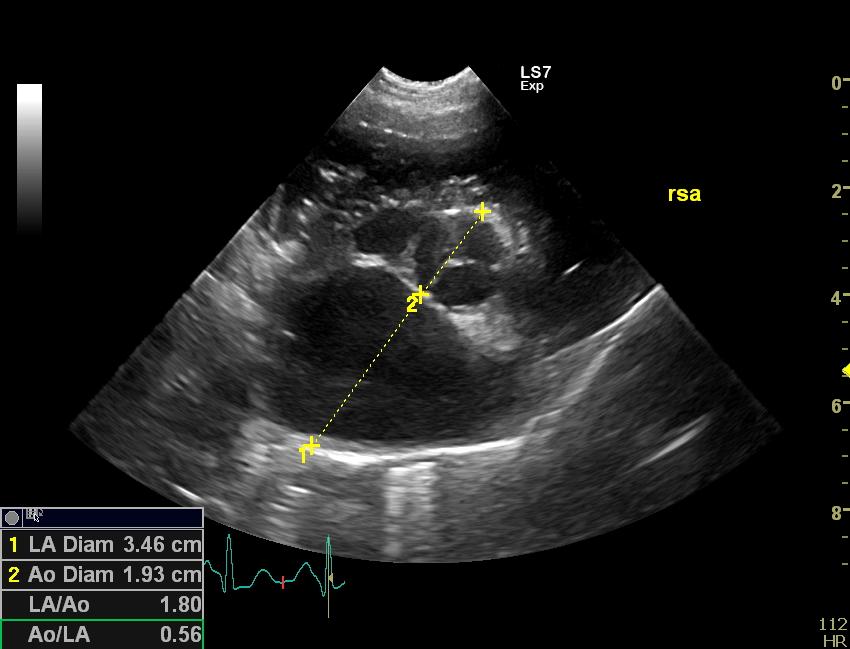
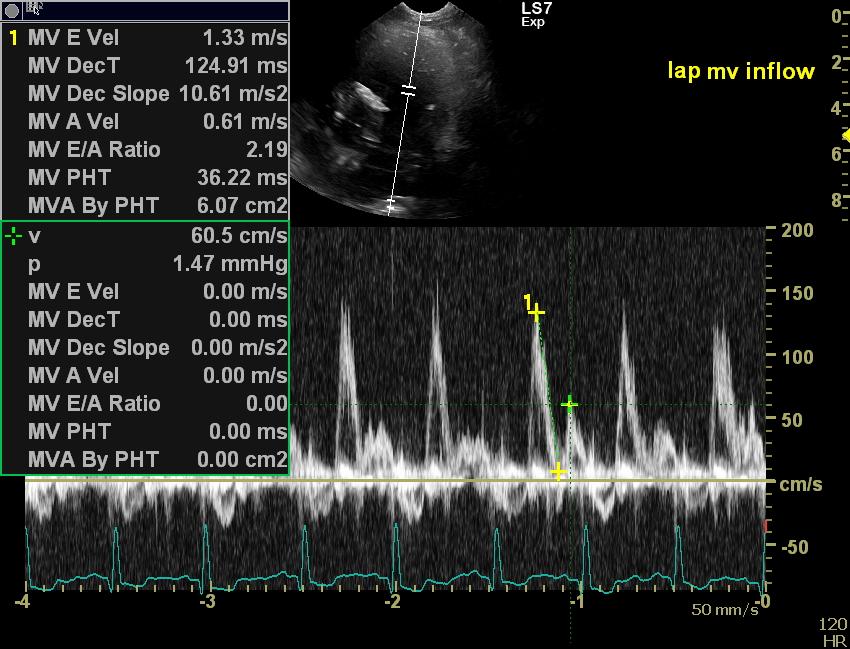
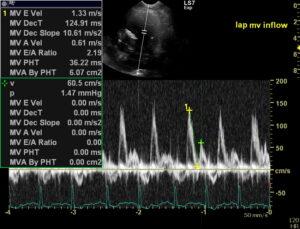
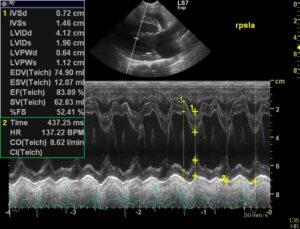
Mid-September: represented not doing well. A 5/6 murmur with a palpable thrill was noted in the left chest (previously 3/6 at the earlier exam and in April) with mild crackles noted on auscultation. Heart rate was 150bpm with dyspnea and the dog was hypertensive. Ultrasound revealed moderate severe eccentric hypertrophy of the LV with moderate left atrial enlargement. Both AMV and PMV leaflets were thickened and irregular with what appeared to be vegetative growths consistent with vegetative endocarditis. The aortic valve was normal in function and appearance. A restrictive mitral inflow was noted. Tricuspid regurgitation velocity suggested mild pulmonary hypertension most likely from the downstream cause. Treatment with Pimobendin 2.5mg BID, Furosemide 2mg/Kg BID and Benazipril 10mg SID was started. Enrofloxacin was added to the antibiotic regimen. Blood and urine culture were negative. Antibiotic therapy will continue for at least two months and possible three along with follow up blood work.
Follow up in October – clinical improvement with a respiratory rate of 12-23/minute, eating kibble as long as she was enticed and readily ate treats and home cooked food. She gained 1 KG of bodyweight. Activity was good for basic living but owner had removed toys that would cause her physical exertion. A 5/6 murmur was still present with a palpable thrill. Ultrasound revealed similar left ventricle and left atrium findings along with vegetative changes present on MV leaflets. TV regurgitation velocity was slightly decreased suggesting normal right sided pressure. Mitral regurgitation was still severe. The pressure gradient across the MV was 127mmHg which was similar to the NIBP measure of 132-134 mmHg. A restrictive mitral inflow profile was still noted. Mitral E velocity was similar at 1.27m/s. Heart rate was 109-136 bpm.
Question:
Significant clinical improvement is noted with the present course of therapy as well as some small positive echo changes (slightly decreased E velocity although E:A is still restrictive, normal TV regurge pressure gradient, normal blood pressure and normal heart rate). Should treatment be based on clinical improvement alone or further tweaked based on echo findings (addition of spironolactone to antagonize aldosterone further, consider use of low dose amlodipine, altering pimobendin or furosemide dose and or frequency etc.) to further improve the echo “numbers”? Should you look to try and decrease the LV and LA size as well as move the E vel closer to 1m/s with a change in dosage or addition of another drug if clinically the dog is doing well? I’m not sure what positive echo changes would typically be expected with the present improved clinical signs with these drugs on board. Before echo and measurements, response to therapy was key lol. I’m assuming that is still the case??
Thanks for having a read and a look!
Comments
Hi!
Interesting case! I would always monitor WBC/PLT and CRP and would continue antibiotic treatment at least for 12 weeks if the patients recovers clinically and based on blood testing. Re E/A-waves: E-waves of 1.3 m/s are mostly not associated with present CHF. I would guide treatment of mitral insufficiency mainly on clinical parameters and would not try to get the E wave down to 1 m/s. this would need very high doses of diuretics and possibly kill the kidneys. I would also repeat blood cultures/urine cultures at least once after discontinuation of AB treatment. And I would test for Bartonella as well. Hope this helps Peter