– 6 year old MN German Shephard cross presented for diarrhea, decreased appetite and mild weight loss BCS 3/5
– 6 year old MN German Shephard cross presented for diarrhea, decreased appetite and mild weight loss BCS 3/5
– hypoalbuminemia, low TP, hypocalcemia on biochem
– CBC wnl, resting cortosol normal, cPLI normal, urine pro:crea normal
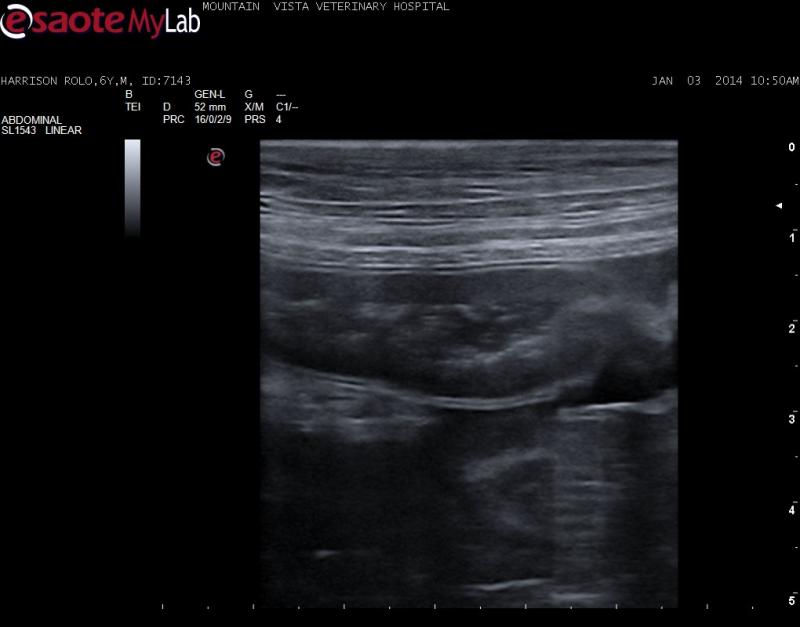
– u/s findings include abdominal and plueral effusion, pancreatic edema, thickended SI mucosal layer with mucosal stippling (mucosal striations were not appreciated but my linear probe is acting funny lately and I am getting it looked at). No lymphadenopathy
– endoscopic intestinal biopsy was recommended but declined by the owner so left to treat medically
DDx: lymphangiectasia, neoplasia (lymphoma), IBD
– started in RC low fat diet, 1 mg/kg pred BID, tylosin, weekly B12 injections to start but think I should add another immunosuppressive – any experience here with chlorambucil?

Comments
see attached typical
see attached typical yorkie with ple and stippling/striations on the microconvex and a typical PLE on linear.
Search the basic search for PLE and there will be many of them as well.
http://sonopath.com/members/case-studies/search
I Like plasma transusion to help keep the albumin > 2.0 as bad things happen when its under 1.5 like thromboembolic disease and if there is a need for sx then they won’t heal well. Plasma gets a jump start and buys time. Purina HA or Royal canine HP, cover for parasites, metronidazole and plasma expanders as needed and of course prednisone. PLE can occur as paraneoplastic so ensure no LSA. You can get fancy and do a corn oil test and scope for duodenal bx to confirm the dx.
See this unedited partial excerpt for the curbside guide coming out in the next couple of months on PLE:
Diagnosis: Typical diagnostics for protein losing enteropathy (PLE) include the clinical profile of hypoalbuminemia (but may also be within normal serum levels), a sonogram with suggestive intestinal wall prominence and mucosal striations noted, and clinical signs of vomiting, weight loss, diarrhea. Be warned some cases can have a lack of GI signs altogether and no weight loss. PLE is preferably definitively diagnosed by full thickness or endoscopy guided biopsies after feeding a fatty meal the night before in order to dilate lacteals to adequately diagnose lymphangiectasia. PLE can be associated with:
Often GI blood loss may occur potentially caused by lymphosarcoma, ulcerative disease, or intussusception. A dynamic sonogram testing procedure feeding corn oil (0.5-1 cc/kg) 45 minutes prior to the sonogram of an NPO patient will enhance the presence of mucosal striations in the small intestine during the sonogram. This is a reliable test founded by Marks et al. at UC Davis (NAVC 2011).
Endoscopy both anterior and posterior approaches are ideal in order to access the stomach/duodenum in the former case and colon/ileum in the latter in order to maximize the biopsy information. However, this will not detect transmural disease such as lymphoma affecting the muscularis and submucosa that are not typically obtained readily via endoscopy. Ultrasound evaluation of the GI tract can help decide whether the pathology is luminal, and available for sampling through endoscopy, or mural and necessitating US-guided FNA or core biopsy or surgical biopsy ideally guided by intra-operative ultrasound. More information regarding intra-operative ultrasound may be found in “resources” at http://www.sonopath.com.
B12, Folate, Ionized calcium, ionized magnesium and antithrombin levels should all be measured in the clinical PLE patient and levels should be corrected with Calcium gluconate (50-150 mg/kg Iv over 12-24 hours) or 1 tablet extra strength Tums (300 mg calcium) PO SID to TID as needed to maintain normal calcium levels over 3-4 weeks. Mg sulphate (1mEq/kg/day IV) or MgOxide 10-20 mg/kg PO BID (Milk of magnesia) may be utilized for magnesium supplementation but milk of magnesia may cause diarrhea.
Yorkshire Terriers are 10X more likely to develop IBD and 9X more likely to suffer hypocalcemia and hypomagnesemia with IBD. Therefore magnesium and calcium supplementation may be in order.
Other differentials for Hypoalbuminemia include:
Hypocalcemia may be present owing to albumen loss (carrier proteins). If depressed cholesterol is also present with hypoalbuminemia then either liver failure or PLE should be suspected. Hypocalcemia may also be an issue with PLE and general causes of Hypoalbuminemia.
Hypocalcemia differentials include:
Treatment: Given that a significant fraction of PLE cases are caused by a food allergy causing IBD, then lymphangiectasia and leading to PLE, Purina HA diet should be fed. This diet is low (not restricted in fat) in fat; low enough to use for lymphangiectasia cases. Plus, it is hydrolyzed, meaning there is nothing in which the body can respond antigenically. No other hydrolyzed or novel protein diets are as low in fat. (Z/D, RC, HP, and IVD diets are moderately high in fat).
It is a good idea to rule out parasitism and/or utilizing empirical treatment with Fenbendazole 50 mg/kg SID for 5 days & repeat in 2 weeks combined with Metronidazole 15mg/kg BID for 10 days. Also ruling out neoplasia with FNA or biopsy, if a target is available or full thickness may be performed. Occasionally GI lymphoma or mast cell disease may be emerging in these cases.
Feeding normal levels of fat with lymphangiectasia patients causes further dilation of the lacteals with rupture, exacerbating protein losses. Many recommend a low fat diet with lymphangiectasia, however, if the primary cause was a food allergy, this recommendation could be counterproductive.
Feed Purina HA for a few weeks and monitor total protein and albumin. If the levels are still low, I would transition to a novel protein diet that is ultra restricted in fat (ostrich, kangaroo, crab). Since none exist commercially, the diet would have to be homemade, which can be expensive for the owner to make. This largest challenge is to make the diet balanced. Homemade diet formulations created through a nutritional consultation is recommended.
Low dose lasix (1-2 mg/kg BID) and/or spironolactone (2-4 mg/kg BID) may be utilized for ascites until oncotic pressures are restored with a colloid or plasma therapy. Abdominocentesis should be utilized only to keep the patient comfortable owing to excessive abdominal distention. Excessive drainage will cause further depletion of the protein supply that we are trying to restore.
B12 supplementation of 250-1,000 ug (cat/small dog lower end, Large breed higher end dose or 1/4cc-1cc) SC weekly x 6 weeks would be recommended owing to loss of B12 in the ileum regardless of serum levels.
Aspirin therapy is suggested (1 mg/kg sid) to assist in potential thromboembolic episodes that are the often the source of sudden death in these cases owing to antithrombin III loss. This dose will not cause side effects in GI tract or elsewhere.
Azothiaprine or cyclosporine may also be considered for refractory cases.
In a last ditch effort if this doesn’t work and biopsies are still not possible then a prednisone trial would be in order. I always prefer utilizing cortisones in these patients based on biopsy results but realize that this is not feasible in many cases.
see attached typical
see attached typical yorkie with ple and stippling/striations on the microconvex and a typical PLE on linear.
Search the basic search for PLE and there will be many of them as well.
http://sonopath.com/members/case-studies/search
I Like plasma transusion to help keep the albumin > 2.0 as bad things happen when its under 1.5 like thromboembolic disease and if there is a need for sx then they won’t heal well. Plasma gets a jump start and buys time. Purina HA or Royal canine HP, cover for parasites, metronidazole and plasma expanders as needed and of course prednisone. PLE can occur as paraneoplastic so ensure no LSA. You can get fancy and do a corn oil test and scope for duodenal bx to confirm the dx.
See this unedited partial excerpt for the curbside guide coming out in the next couple of months on PLE:
Diagnosis: Typical diagnostics for protein losing enteropathy (PLE) include the clinical profile of hypoalbuminemia (but may also be within normal serum levels), a sonogram with suggestive intestinal wall prominence and mucosal striations noted, and clinical signs of vomiting, weight loss, diarrhea. Be warned some cases can have a lack of GI signs altogether and no weight loss. PLE is preferably definitively diagnosed by full thickness or endoscopy guided biopsies after feeding a fatty meal the night before in order to dilate lacteals to adequately diagnose lymphangiectasia. PLE can be associated with:
Often GI blood loss may occur potentially caused by lymphosarcoma, ulcerative disease, or intussusception. A dynamic sonogram testing procedure feeding corn oil (0.5-1 cc/kg) 45 minutes prior to the sonogram of an NPO patient will enhance the presence of mucosal striations in the small intestine during the sonogram. This is a reliable test founded by Marks et al. at UC Davis (NAVC 2011).
Endoscopy both anterior and posterior approaches are ideal in order to access the stomach/duodenum in the former case and colon/ileum in the latter in order to maximize the biopsy information. However, this will not detect transmural disease such as lymphoma affecting the muscularis and submucosa that are not typically obtained readily via endoscopy. Ultrasound evaluation of the GI tract can help decide whether the pathology is luminal, and available for sampling through endoscopy, or mural and necessitating US-guided FNA or core biopsy or surgical biopsy ideally guided by intra-operative ultrasound. More information regarding intra-operative ultrasound may be found in “resources” at http://www.sonopath.com.
B12, Folate, Ionized calcium, ionized magnesium and antithrombin levels should all be measured in the clinical PLE patient and levels should be corrected with Calcium gluconate (50-150 mg/kg Iv over 12-24 hours) or 1 tablet extra strength Tums (300 mg calcium) PO SID to TID as needed to maintain normal calcium levels over 3-4 weeks. Mg sulphate (1mEq/kg/day IV) or MgOxide 10-20 mg/kg PO BID (Milk of magnesia) may be utilized for magnesium supplementation but milk of magnesia may cause diarrhea.
Yorkshire Terriers are 10X more likely to develop IBD and 9X more likely to suffer hypocalcemia and hypomagnesemia with IBD. Therefore magnesium and calcium supplementation may be in order.
Other differentials for Hypoalbuminemia include:
Hypocalcemia may be present owing to albumen loss (carrier proteins). If depressed cholesterol is also present with hypoalbuminemia then either liver failure or PLE should be suspected. Hypocalcemia may also be an issue with PLE and general causes of Hypoalbuminemia.
Hypocalcemia differentials include:
Treatment: Given that a significant fraction of PLE cases are caused by a food allergy causing IBD, then lymphangiectasia and leading to PLE, Purina HA diet should be fed. This diet is low (not restricted in fat) in fat; low enough to use for lymphangiectasia cases. Plus, it is hydrolyzed, meaning there is nothing in which the body can respond antigenically. No other hydrolyzed or novel protein diets are as low in fat. (Z/D, RC, HP, and IVD diets are moderately high in fat).
It is a good idea to rule out parasitism and/or utilizing empirical treatment with Fenbendazole 50 mg/kg SID for 5 days & repeat in 2 weeks combined with Metronidazole 15mg/kg BID for 10 days. Also ruling out neoplasia with FNA or biopsy, if a target is available or full thickness may be performed. Occasionally GI lymphoma or mast cell disease may be emerging in these cases.
Feeding normal levels of fat with lymphangiectasia patients causes further dilation of the lacteals with rupture, exacerbating protein losses. Many recommend a low fat diet with lymphangiectasia, however, if the primary cause was a food allergy, this recommendation could be counterproductive.
Feed Purina HA for a few weeks and monitor total protein and albumin. If the levels are still low, I would transition to a novel protein diet that is ultra restricted in fat (ostrich, kangaroo, crab). Since none exist commercially, the diet would have to be homemade, which can be expensive for the owner to make. This largest challenge is to make the diet balanced. Homemade diet formulations created through a nutritional consultation is recommended.
Low dose lasix (1-2 mg/kg BID) and/or spironolactone (2-4 mg/kg BID) may be utilized for ascites until oncotic pressures are restored with a colloid or plasma therapy. Abdominocentesis should be utilized only to keep the patient comfortable owing to excessive abdominal distention. Excessive drainage will cause further depletion of the protein supply that we are trying to restore.
B12 supplementation of 250-1,000 ug (cat/small dog lower end, Large breed higher end dose or 1/4cc-1cc) SC weekly x 6 weeks would be recommended owing to loss of B12 in the ileum regardless of serum levels.
Aspirin therapy is suggested (1 mg/kg sid) to assist in potential thromboembolic episodes that are the often the source of sudden death in these cases owing to antithrombin III loss. This dose will not cause side effects in GI tract or elsewhere.
Azothiaprine or cyclosporine may also be considered for refractory cases.
In a last ditch effort if this doesn’t work and biopsies are still not possible then a prednisone trial would be in order. I always prefer utilizing cortisones in these patients based on biopsy results but realize that this is not feasible in many cases.
Thanks for the info! I also
Thanks for the info! I also found this recent study but don’t know how much, if anyone is trying chlorambucil in their patients.
Comparison of a chlorambucil-prednisolone combination with an azathioprine-prednisolone combination for treatment of chronic enteropathy with concurrent protein-losing enteropathy in dogs: 27 cases (2007-2010).
Author information
Abstract
OBJECTIVE:
To compare treatment protocols for chronic enteropathy and concurrent protein-losing enteropathy that used prednisolone in conjunction with either azathioprine or chlorambucil in dogs.
DESIGN:
Retrospective case series.
ANIMALS:
27 dogs.
PROCEDURES:
All dogs had hypoalbuminemia (serum albumin concentration, < 18.0 g/L) and chronic enteropathy as diagnosed via complete gastrointestinal tract investigations including intestinal biopsy. Dogs received either an azathioprine-prednisolone combination (group A; n = 13) or a chlorambucil-prednisolone combination (group C; 14). Response to treatment was assessed by evaluation of body weight gain, serum albumin concentration, and duration of primary treatment.
RESULTS:
No significant pretreatment differences were detected between groups for any baseline variable (signalment and weight), clinicopathologic variable (albumin, cobalamin, and folate concentrations), or histopathologic findings. After treatment, serum albumin concentration and weight gain were significantly greater in group C. Median survival time for group A dogs was 30 days (95% confidence interval, 15 to 45 days) and was not reached for group C dogs. Duration of primary treatment was positively associated with the histopathologic presence of mild lacteal dilatation and use of a chlorambucil-prednisolone combination.
CONCLUSIONS AND CLINICAL RELEVANCE:
Results suggested that a chlorambucil-prednisolone protocol is more efficacious for treatment of chronic enteropathy and concurrent protein-losing enteropathy, compared with an azathioprine-prednisolone combination. Given these findings, a prospective randomized clinical trial is warranted.
Thanks for the info! I also
Thanks for the info! I also found this recent study but don’t know how much, if anyone is trying chlorambucil in their patients.
Comparison of a chlorambucil-prednisolone combination with an azathioprine-prednisolone combination for treatment of chronic enteropathy with concurrent protein-losing enteropathy in dogs: 27 cases (2007-2010).
Author information
Abstract
OBJECTIVE:
To compare treatment protocols for chronic enteropathy and concurrent protein-losing enteropathy that used prednisolone in conjunction with either azathioprine or chlorambucil in dogs.
DESIGN:
Retrospective case series.
ANIMALS:
27 dogs.
PROCEDURES:
All dogs had hypoalbuminemia (serum albumin concentration, < 18.0 g/L) and chronic enteropathy as diagnosed via complete gastrointestinal tract investigations including intestinal biopsy. Dogs received either an azathioprine-prednisolone combination (group A; n = 13) or a chlorambucil-prednisolone combination (group C; 14). Response to treatment was assessed by evaluation of body weight gain, serum albumin concentration, and duration of primary treatment.
RESULTS:
No significant pretreatment differences were detected between groups for any baseline variable (signalment and weight), clinicopathologic variable (albumin, cobalamin, and folate concentrations), or histopathologic findings. After treatment, serum albumin concentration and weight gain were significantly greater in group C. Median survival time for group A dogs was 30 days (95% confidence interval, 15 to 45 days) and was not reached for group C dogs. Duration of primary treatment was positively associated with the histopathologic presence of mild lacteal dilatation and use of a chlorambucil-prednisolone combination.
CONCLUSIONS AND CLINICAL RELEVANCE:
Results suggested that a chlorambucil-prednisolone protocol is more efficacious for treatment of chronic enteropathy and concurrent protein-losing enteropathy, compared with an azathioprine-prednisolone combination. Given these findings, a prospective randomized clinical trial is warranted.
It makes sense and leukeran
It makes sense and leukeran is quite tolerable… dont know if its necessary but maybe for refractive cases..
It makes sense and leukeran
It makes sense and leukeran is quite tolerable… dont know if its necessary but maybe for refractive cases..
I have used chlorambucil
I have used chlorambucil combined with cyclosporine in refractory cases with good results and minimal side effects.
I have used chlorambucil
I have used chlorambucil combined with cyclosporine in refractory cases with good results and minimal side effects.