- 7 year old JRT – weight loss, inappetance, diarrhoea
- Bloods: mild anaemia, mild hypoalbuminaemia, mild hyperglobulinaemia, neutrophilic leukocytosis (no smear)
- No response to antibiotics
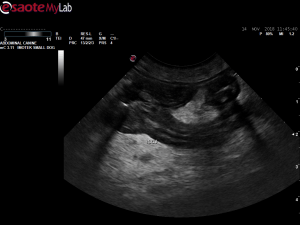
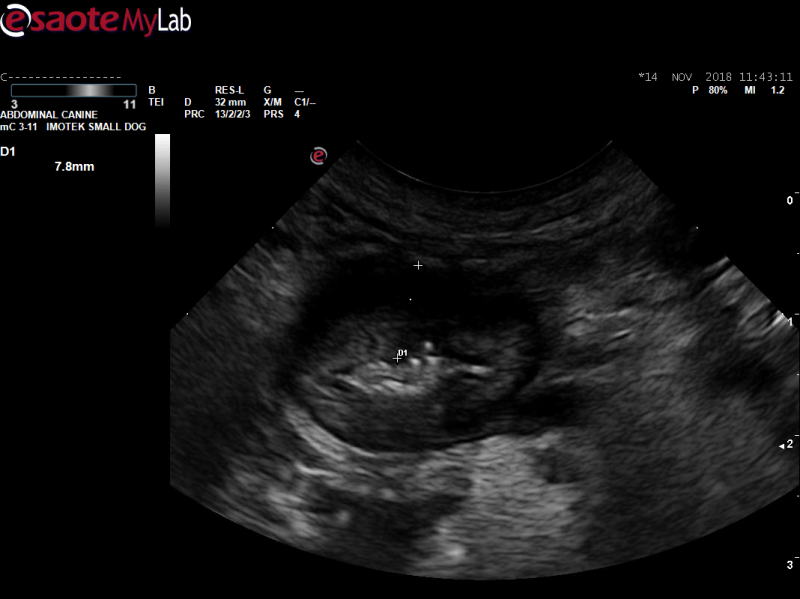
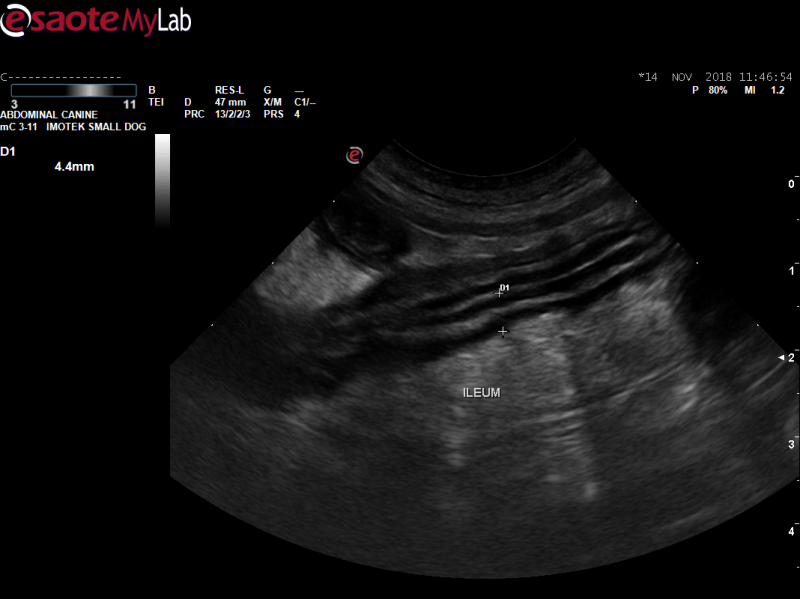
- Scan: thickened large intestine esp proximal section with loss of layering, altered layering of ileum, rounded hypoechoic local lymph nodes with surrounding steatits
- I felt like I got good FNAs of thickened intestine and LN, cellularity high and cell preservation good on both
- 7 year old JRT – weight loss, inappetance, diarrhoea
- Bloods: mild anaemia, mild hypoalbuminaemia, mild hyperglobulinaemia, neutrophilic leukocytosis (no smear)
- No response to antibiotics
- Scan: thickened large intestine esp proximal section with loss of layering, altered layering of ileum, rounded hypoechoic local lymph nodes with surrounding steatits
- I felt like I got good FNAs of thickened intestine and LN, cellularity high and cell preservation good on both
- Cytology results: LN – reactive hyperplasia, LI – iatrogenic haemorrhage with more leukocytes than expected for blood contamination alone. Non-degenerate neutrophils predominate. The lymphocytes are small and well differentiated. Larger lymphoid cells or plasma cells, intestinal epithelial cells, other cell types or microorganisms not found.
- I was strongly suspicious for lymphoma. What do you think is causing this and how would you proceed?
Comments
I think biopsies would be
I think biopsies would be essential in this case to get histopath diagnosis and to guide treatment. Etiologies for the colon, in my opinion, would include severe inflammatory, infectious, granulomatous or ulcerative colitis and neoplasia. I dont think we can rule out neoplasia based on the FNA results. If biopsies are elected and pending initial histopath, FISH (Fluorescent In Situ Hybridization) for bacteria assessent may be needed. Im not sure of this test is available in Europe, but Cornell runs it.
The anemia may be secondery to chronic disease or possible chronic GI bleeding if there is evidence of melena.
May be reaching here, but the predominance of non degenerative neutrophils on the cytology may indicate a neutrophilic or suppurative colitis.
I would consider a 4-6 week course of Enrofloxacin if it wasn’t in the initial antibiotic treatment to cover for E. coli. A limited antigenic or hydrolyzed diet and broad spectrum antiparasite treatment, if not done, as well.
Thank you. I was expecting
Thank you. I was expecting anans weer from the FNA so just frustrating. Not sure if owners will go fo rf biopsy but will certainly trial treatment.