A 3-year-old MN Jack Russell Terrier with history of elevated ALT activity; treated with Ursodial in Japan, was presented for an initial visit. Physical examination was unremarkable and the owners were advised to stop giving the Ursodial. The patient was presented for vomiting for 3 days shortly after his initial visit. Physical examination and survey radiographs were both within normal limits. Blood chemistry revealed moderately elevated ALT activity and elevated pre-and post-prandial bile acids (175.9 and 449.1 umol/L, respectively).
A 3-year-old MN Jack Russell Terrier with history of elevated ALT activity; treated with Ursodial in Japan, was presented for an initial visit. Physical examination was unremarkable and the owners were advised to stop giving the Ursodial. The patient was presented for vomiting for 3 days shortly after his initial visit. Physical examination and survey radiographs were both within normal limits. Blood chemistry revealed moderately elevated ALT activity and elevated pre-and post-prandial bile acids (175.9 and 449.1 umol/L, respectively). The patient was treated with Pepcid and Cerenia, and discharged with Gastro calm. The patient was recommended for treatment with Denamarin, Flagyl, Lactulose, and a low protein liver diet.
Case Study
03_00176 Jeter G Splenoazygos shunt and microvascular dysplasia *Oct 2012 COM*
DX
Sonographic Differential Diagnosis
Extra hepatic shunt bypassing the vena cava consistent with splenoazygos shunt. Surgically correctable. Potential for concurrent microvascular dysplasia.
Image Interpretation
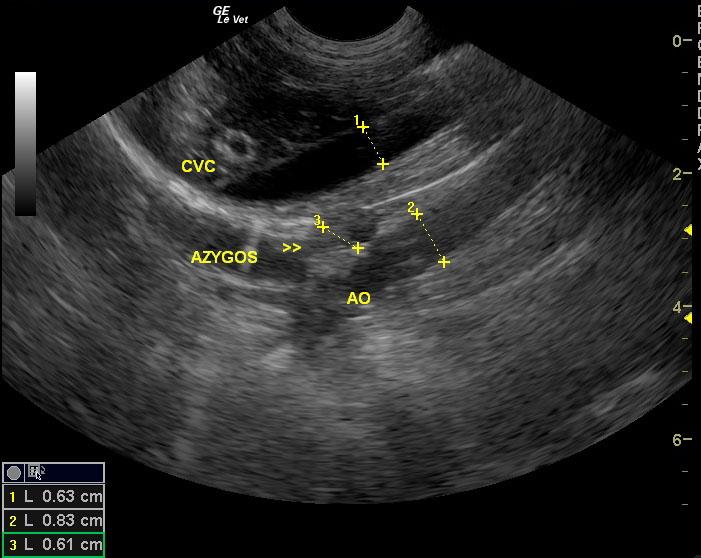
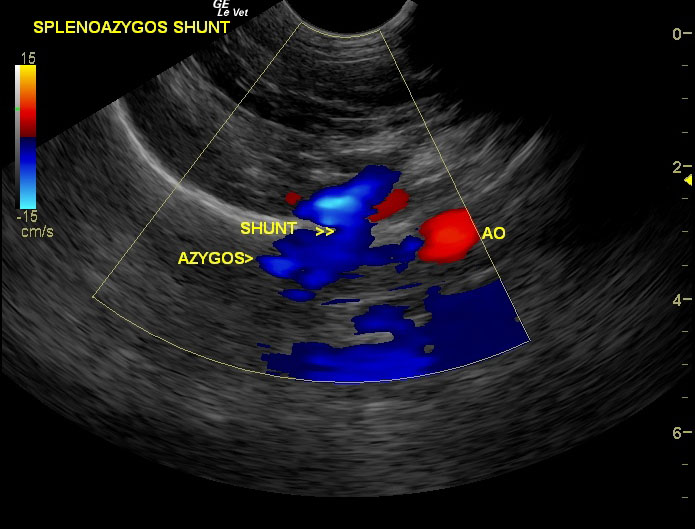
Image 1: Small bladder calculi are present with only slight shadowing (+ predictive shunt factor). Image 2: The right kidney does not present any calculi but does reveal and interstitial nephrosis pattern (- predictive factor). Image 3: Mild microhepatica is evident in this long axis view where the diaphragm takes a horizontal angle. Minor Gb distention is present which is normal for a fasted patient. (microhepatica + predictive factor). Image 4: Transverse view of the liver demonstrating only 3.5 cm of hepatic parenchyma further supporting microhepatica. Image 5: Portal hepatis demonstrating a vertical aberrant blue vessel (direction dorsally away from probe; BART= Blue Away Red Toward). The portal vein in the near field prior to the vertical vessel is a 1:1 ratio with the vena cava in the far field. The vena cava maintains a constant volume cranially. Image 6: Following the aberrant blue vessel dorsally we see the horizontal vena cava that does not increase in volume and has constant non turbulent flow. Image 7: Further dorsally toward the diaphragm the vertical blue vessel enters into the diaphragmatic inlet near the vena cava without creating turbulent flow in the cava. Image 8: Long axis oblique view of the vena cava (near field) and the aorta (far field) as they enter into the diaphragm with a 1:1 ratio of vena cava/aorta indicating that the aberrant vessel does not enter into the vena cava since there is no excessive volume. A third anechoic vessel is “sandwiched” cranial to the diaphragm between the vena cava and aorta. Image 9: Still image demonstrating the 1:1 vena cava/aorta ratio and the splenoazygos shunt as it enters the diaphragm creating a “double aorta” effect. Image 10: Color flow evidencing the “double aorta.” Image 11: Splenoazygos shunt (blue) as it enters the diaphragm at the level of the aorta and esophageal inlet. Image 12: Azygos shunt “poster.” Compare these findings with the negative shunt hunt from Case of the month, July 2010. (http://www.sonopath.com/COM_1007.html)
Outcome
The patient was recommended for urinary bladder lavage, ameroid constrictive placement upon the extra-hepatic spleno-azygos shunt, and concurrent liver biopsy. On exploratory surgery, a large splenoazygos shunt was identified and attenuated with an ameroid constrictor, liver biopsies were taken, a cystotomy was performed, and a culture from the bladder wall was obtained. The patient was discharged with Clavamox, Tramadol, and recommended for a special low protein liver diet. At last communication the owner reported the patient doing well.
Comments
November 2010 case of the month Title: The Shunt Hunt Revisited. A Jack Russel Terrier from Yankee nation has to be named “Jeter.” But does “Jeter” have a shunt and can it be corrected in time for the playoffs? Case Imaged by Eric Lindquist DMV, DABVP. Patient managed by Abe Van Beveren DVM of Madison VH, Madison, NJ & Tom Scavelli & staff at Garden State VS, Tinton Falls, NJ, USA. Special thanks to Dr. Abe Van Beveren & staff at Madison Veterinary Hospital, Madison, NJ, USA (http://www.vcahospitals.com/madison) and Dr. Tom Scavelli & Staff at Garden State Veterinary Specialists, Tinton Falls, NJ, USA (http://www.gsvs.org/) for the medical and surgical management of this case. Regarding shunt diagnostics via ultrasound and other studies, see our ECVIM abstract from Toulouse, France 2010 in our resources tab at SonoPath.com http://www.sonopath.com/resources.html
Clinical Differential Diagnosis
Vomition – infectious (viral, bacterial, helminths), diet, toxins, garbage disease, liver disease. Liver disease – congenital (MVD, PSS), cirrhosis
Sampling
Full-thickness surgical biopsies of the liver showed hepatic microvascular dysplasia. Culture of the bladder wall yielded no growth.