History
This 7-year-old MN DSH presented for dysuria and a history of persistent UTI. This presentation progressed into episodes of vomiting, weight loss and “not doing right” as reported by the owner over a 1 month period. The physical exam revealed a palpable mass in the cranial abdomen that was confirmed by radiographs and positioned caudal to the stomach. The CBC was normal. Blood chemistry was normal except for a minor globulin elevation. Urinalysis (free catch): PH 6.0, USG 1.032, appearance cloudy, leukocytes moderate, protein 100+, epithelia, and bacteria (cocci).
Clinical Differential Diagnosis
UTI/pyelonephritis, urolithiasis, pancreatitis, neoplasia, IBD, infectious disease.
Image Interpretation
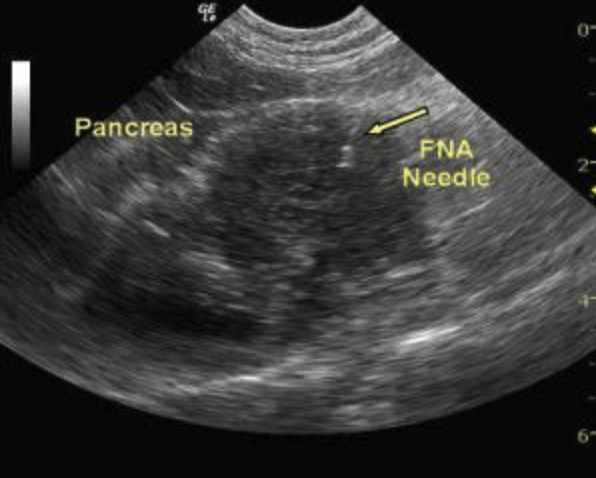
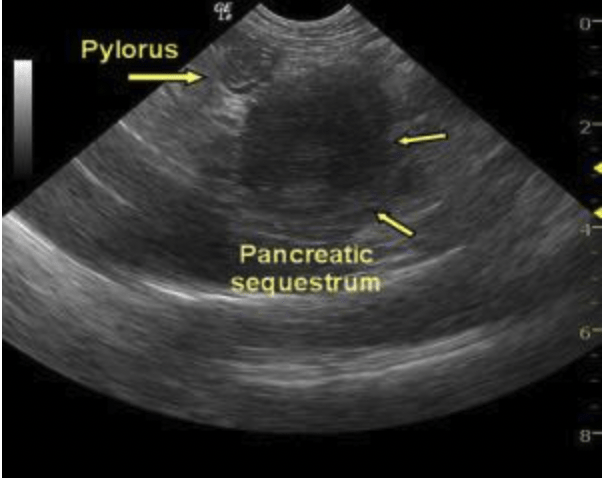
Image 1: A well-circumscribed, hypoechoic mass positioned within the region of the body of the pancreas. Image 2: The mesentery and omentum boarding the pancreas is mildly echogenic and may be adhered. The echogenic linear focus at the 1 o’clock position represents a 22-gauge needle.
Sonographic Differential Diagnosis
Suspect chronic pancreatitis with mild peri-pancratic fibrosis, inflammation and adhesions with an accompanying avascular mass. Differentials for the mass include abscessing or necrotizing neoplasm or focal pancreatitis, sequestration.
Sampling
22g US-guided FNA was performed on variable hypoechoic portions of the pancreas. Cytology: Marked pancreatitis/steatitis/necrosis. No evidence of neoplasia was found.
Outcome
Bartonella henselae. The patient has been thriving for over a year but did recently have a similar but less dramatic clinical presentation that responded to hospitalization and similar treatment.
Comments
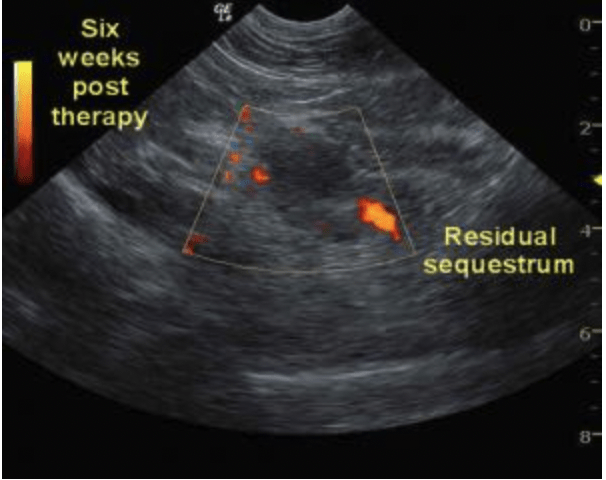
The patient responded well to IV fluid support, plasma expander therapy and endovenous antibiotics. Out-patient therapy included multimodal antibiotics and nutritional support. A single dose of dexamethazone was also administered to reduce inflammation. The patient was essentially asymptomatic for 5 weeks and antibiotic therapy was stopped. One week later the patient again presented for lethargy and anorexia. A follow-up sonogram was performed with power flow Doppler 6 weeks post therapy. Image 3: The residual mass is continuous with the right limb which is mildly enlarged, hypoechoic, with evidence of normal perfusion noted with power flow Doppler. A concurrent splenic abscess was found on sonogram that most likely contributed to the symptoms. Tom was again hospitalized and discharged 3 days later responding to multimodal antibiotic therapy. Surgical biopsies were taken 2 months later by owner request to further define the persistent pathology. The patient was essentially stable at that time. At this time the owners wished to further define this pathology with surgical histopathology: Pancreatic nodular hyperplasia, severe chronic lymphoplasmacytic cholangiohepatitis, Mild, chronic, lymphoplasmacytic enteritis, moderate, chronic, fibrosing inflammation and splenic adhesion. Mild chronic, proliferative, mesenteric lymphadenopathy. Mild, chronic, ulcerative, fibrosing cystitis. This is typical hisopathology of a “triad” cat. The pancreatic nodular hyperplasia would be consistent with sequelae from chronic pancreatitis. The patient recovered uneventfully and was stable without medication 2 months post exploratory surgery. Referring Practitioner: Dawn Garro DVM, Pequannock Animal Hospital, Pompton Plains, NJ, USA
Patient Information
Age
Gender
Species
7 Years
Male, Neutered
Feline