A 3-year-old FS Pomeranian dog presented at emergency facility for five episodes of acute vomiting, anorexia, and lethargy. Physical exam found the patient to have a slightly tense, painful abdomen. In-house blood chemistry revealed elevated alkaline phosphatase, hyperphosphatemia, hypercholesterolemia, hyperamylasemia, hyperglycemia, and low chloride. CBC found slightly elevated HCT and eosinopenia. The patient had a positive snap CPL. There were ketones in urine. Patient was admitted for intravenous fluids and supportive care.
A 3-year-old FS Pomeranian dog presented at emergency facility for five episodes of acute vomiting, anorexia, and lethargy. Physical exam found the patient to have a slightly tense, painful abdomen. In-house blood chemistry revealed elevated alkaline phosphatase, hyperphosphatemia, hypercholesterolemia, hyperamylasemia, hyperglycemia, and low chloride. CBC found slightly elevated HCT and eosinopenia. The patient had a positive snap CPL. There were ketones in urine. Patient was admitted for intravenous fluids and supportive care. After 24 hours on fluids, patient was still vomiting a great deal, was febrile, and her amylase level was increasing.
Case Study
Diabetes, pancreatitis, and intestinal adhesions in a 3 year old FS Pomeranian
DX
Sonographic Differential Diagnosis
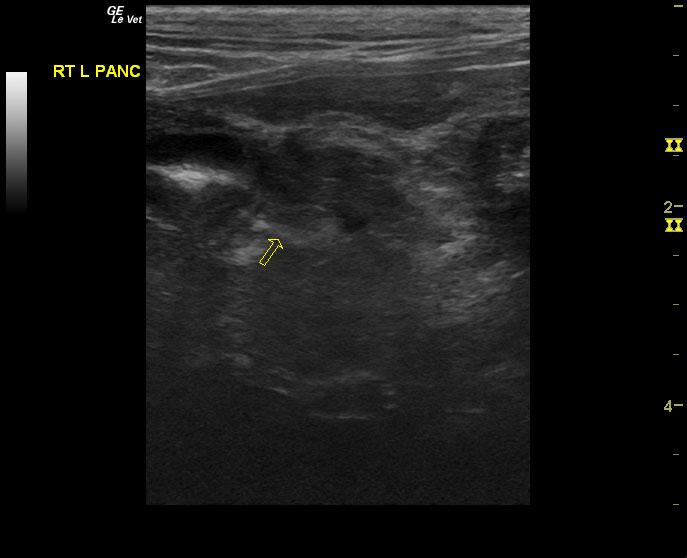
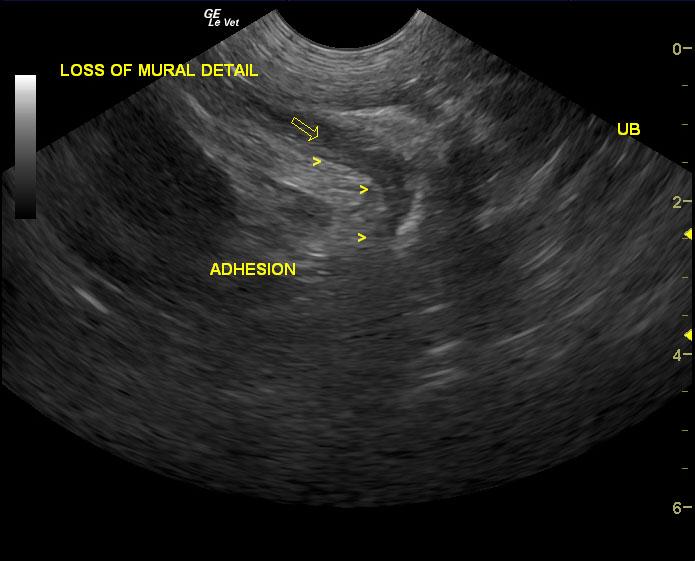
Aggressive pancreatic necrosis in the right limb. Adhesions associated with a separate area of the distal small intestine. These adhesions are most likely due to devitalized bowel which may be caused by transmural intestinal pathology with underlying cause of chronic inflammatory disease or possibly emerging neoplasia though not overtly suspected. Given that the obstructive pattern was demonstrated and the patient was focally painful, bowel infarction or other forms of devitalized bowel is strongly suspected.
Image Interpretation
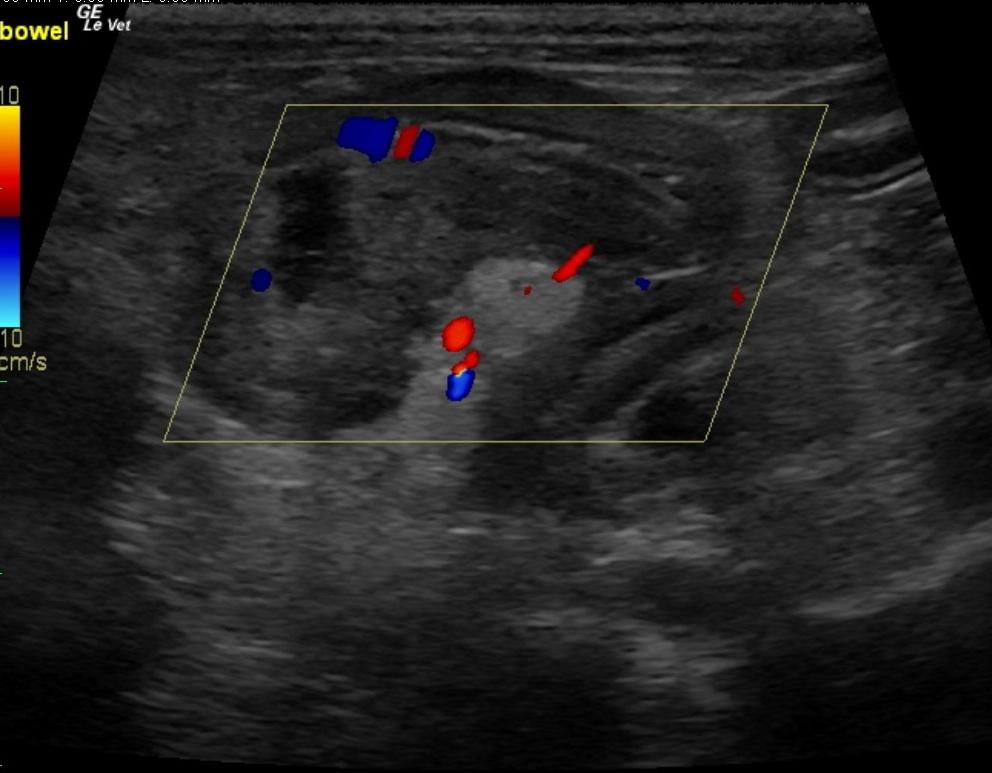
The upper duodenum was very prominent and edematous. The pancreas demonstrated a large amount of mixed, hypoechoic changes. The entire pancreatic portion that appeared affected extended approximately 6-7 cm caudally. Color flow Doppler signals were subnormal in this region, which is suggestive of pancreatic necrosis. There was a minor amount of free fluid that was not sampled. The patient was focally painful on a portion of distal small intestines, which demonstrated diffuse mucosal thickening and omental adhesions. The adhesion pattern to the small intestines was separate from the pancreatitis. Complete absence of peristalsis was noted. Luminal dilation is noted followed by empty small intestine with associated serosal adhesions.
Outcome
Due to potential bowel infarction, exploratory surgery was recommended. A plasma transfusion, Hetastarch, broad-spectrum antibiotics, gastroprotectants, urine culture and sensitivity, and primary urinary tract infection therapy were also advised. Patient was transferred to referral facility and after recheck ultrasound and blood work. Patient was admitted to the hospital for treatment of diabetes and pancreatitis, which included a plasma transfusion. Follow-up ultrasound showed evidence of severe pancreatitis, gastric stasis, and no distinct foreign body. Recheck blood work after 24 hours revealed hyperphosphatemia, low ALT, hypercholesterolemia, low creatinine, and hyperglycemia. Patient was transferred back to RDVM for continued care. Recheck ultrasound a few days later showed pancreatitis and suspicion of possible bowel adhesion/obstruction, and diminished peristaltic activity leading to diminished wall integrity. A diagnostic peritoneal lavage and or exploratory was recommended due to possible bowel infarction or entrapment at the level of the duodenum. After several more days of hospitalization, the patient was discharged to owner with two antibiotics and insulin. Patient presented at referral facility a few days later for another ultrasound to assess pancreatitis and area of bowel under suspicion for possible infarction. Ultrasound showed mild pancreatitis with adjacent peritonitis, and a cystic structure to the right of the cranial abdomen, of unknown origin. Approximately 1 month later, follow ultrasound was performed and found a minor adhesion in the right caudal abdomen, minor low grade residual pancreatitis in right limb or nodular hyperplasia. Continued therapy with the introduction of a hypoallergenic diet with the rotation of protein source every 8 months was advised. TLI result was indicative of normal exocrine pancreatic function.
Comments
No video available on this patient.
Clinical Differential Diagnosis
Diabetic ketoacidosis, pancreatitis, gastritis secondary to dietary indiscretion, infection, GI foreign body, IBD.
Sampling
None taken
Patient Information
Clinical Signs
- Anorexia
- Lethargy
- Vomiting
Exam Finding
- Abdominal Pain
Blood Chemistry
- Alkaline Phosphatase (SAP), High
- Amylase, High
- Chloride, Low
- Cholesterol, High
- Glucose, High
- Phosphorus, High
CBC
- Eosinophils, Low
- Hematocrit, High
Clinical Signs
- Anorexia
- Lethargy
- Vomiting
Special Testing
- cPLI Positive
Urinalysi
- Ketones Present